By Anna Mossing

Isolation stems from a feeling of disconnect, where a physical or emotional distance is often observed. Yet, what about a rhythmic separation?
How do you feel when daylight savings occurs? Or when you deplane from a cross-country red-eye flight? The human body is governed by a circadian rhythm. When your internal clock is skewed due to time changes, you will typically feel disconnected from the rest of the world. A simple solution to calibrate your circadian rhythm is exposure to sunlight. For example, if sunlight isn’t available during a dark Alaskan winter, alternative technologies like light boxes can deliver light at approximately the same wavelengths as sunlight. What if someone is blind and has a complete lack of light detection in their eyes? Neither sunlight nor alternative light therapies would re-set their circadian clock. 80% of blind individuals report sleep disturbance, and over half of totally blind individuals experience a condition called Non-24-Hour Sleep-Wake Disorder, aka “Non-24.”1 This sleep disorder causes a chronic separation from a regular 24-hour circadian rhythm, and isolates the individual from friends, family, and society.1
Allen, A. E. (2019). Circadian rhythms in the blind. Current opinion in behavioral sciences, 30, 73-79.
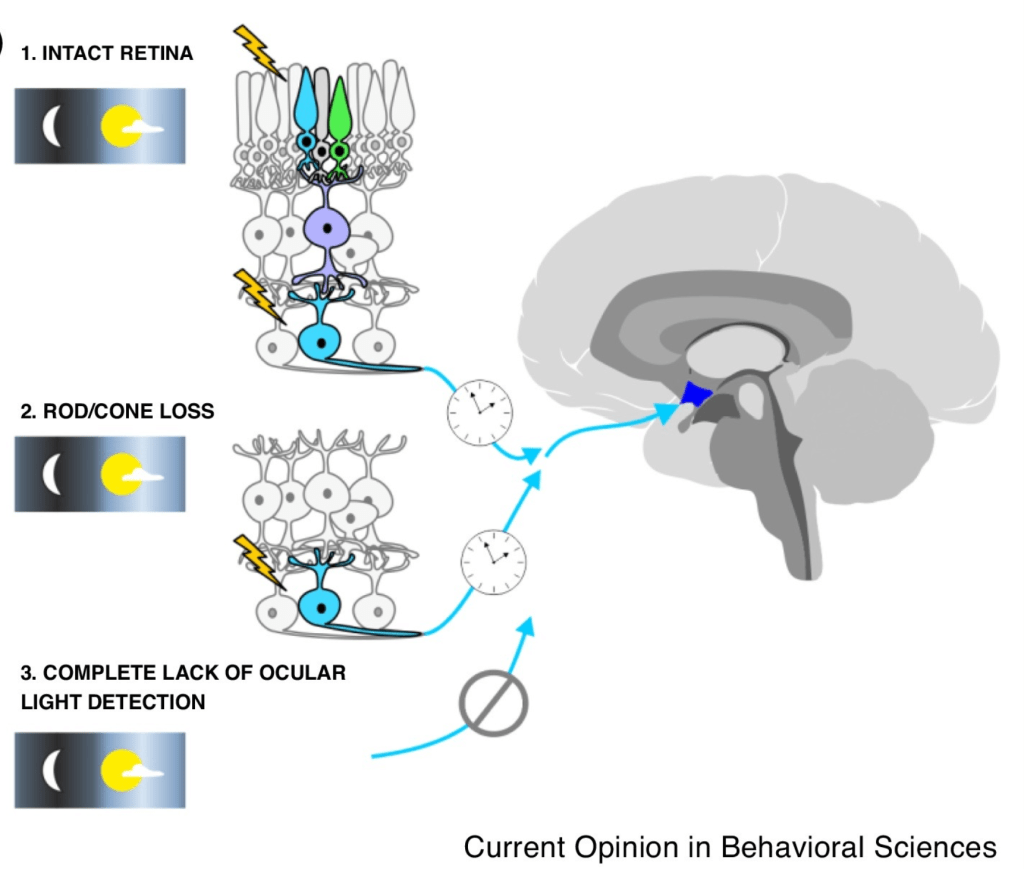
A circadian rhythm is naturally aligned with the Earth’s 24-hour cycle of day and night. The primary cue for synchronizing this rhythm is light, especially sunlight.3 When light hits the retina, it sends signals to the suprachiasmatic nucleus in the brain, which is the master regulator of the circadian rhythm.3 When there is no ocular light detection, no signal is sent and the body cannot synchronize with the day/night schedule.
In 1977, a 28 year-old blind post-graduate student, J.X., struggled to maintain a typical schedule in alignment with his academic and leisure activities.2 Frustrated, and looking for a solution, he set regulated meal and bedtime routines, took stimulant medications, and kept a sleep journal.2 The sleep journal seemed to suggest that he was set on a circadian rhythm longer than 24 hours. To find a solution to this imbalance, Miles entered a medical study. He was encouraged to eat, work, and sleep intuitively, and his alertness, performance, temperature, pulse, and respiration were continuously monitored over a period of 26 days.2
Miles was diagnosed with Non-24 and a 24.9-hour sleep-wake cycle.2 By living according to his own intuitive schedule during the study, Miles did not suffer from excessive tiredness during the day or insomnia at night.2 He felt normal for the for the first time in years. However, his intuitive schedule puts him at odds with the rest of the world.
The second part of the study was specified as an entrainment attempt.2 Miles was scheduled for regimented times of eating, working, and sleeping based on a 24-hour circadian rhythm.2 As weeks progressed with these constraints, he became increasingly restless at night and observably exhausted during the day. Throughout both parts of the sleep study, Miles’ cortisol levels were measured.2 When his cortisol levels were compared to a typical 24-hour circadian rhythm, they seemed sporadic. However, his cortisol levels were a perfect match to a 24.9-hour cycle.2
The best solution for Miles’ well-being was to stick to a 24.9-hour cycle, but his circadian rhythm wasn’t in line with the rest of the world. This created a “scheduling” dilemma for Miles. He had to choose between his own health, and his career advancements and relationships. Navigating this dilemma would impact Miles’ overall quality of life, as he had to choose between quality opportunities and quality health.
Since Non-24 affects a range of people with different backgrounds, ages, and lifestyles, people use a range of methods to manage this disorder and combat its effects. Some use schedule regulation as their primary mode of management, while others use medication.2 Miles coped with his Non 24 through a technique called “free running,” in which he allowed his body to maintain a 24.9-hour cycle.2 While this might decrease his career opportunities and cause tension in friendships, he chose to protect his physical well-being.

(a) Typical sleep-wake schedule. (b) Free running sleep-wake schedule. Allen, A. E. (2019). Circadian rhythms in the blind. Current opinion in behavioral sciences, 30, 73-79.
Mindy, a 60 year-old woman, was born with impaired vision and lost all ocular light detection by the age of 10.8 Once she completely lost light detection, she began struggling with maintaining a regular sleep schedule.8 Eventually she had to stop working due to chronic exhaustion.8 Before being diagnosed with Non-24, Mindy felt hopeless and out of touch with her body.8 Despite being interested in and excited for different events, she missed concerts, lectures, and social gatherings due to her exhaustion or suffered anxiety about falling asleep at events.8 When Mindy was finally diagnosed with Non-24, she experienced hope after years of disappointment. “When I finally got the diagnosis, I couldn’t have been happier. I felt lighter. I felt as though tons of bricks had been lifted off my shoulders, and I felt free. I came home from the doctor feeling like someone had finally heard me,” said Mindy.8 Knowing she has Non-24, Mindy now feels more aware of her body, explaining a new sense of control, “If I am aware then I can plan accordingly.”8
“When I finally got the diagnosis, I couldn’t have been happier… I came home from the doctor feeling like someone had finally heard me.”
As diagnoses of Non-24 became more common, one pharmaceutical company started researching treatments. Between 2010 and 2012, Vanda Pharmaceuticals developed Hetlioz (Tasimelteon) to treat Non-24.4 However, the drug was controversial in practice. During the development of Hetlioz, volunteers dropped out of several clinical trials.4 The drug had a modest success rate, only 29% improvement as compared to 13% in the placebo group.4 Many people have had mixed feelings and experiences with this drug, with some commenting on WebMD reviews. One of these commenters, Ted, was part of a clinical trial for Hetlioz.5 While on the medication, Ted struggled for several nights with nightmares and sleep paralysis, and he also developed urinary tract infections.5 When Ted contacted Vanda Pharmaceuticals about these side effects, he felt they were evasive with their answers and not empathetic.5 Ianto, another reviewer, was prescribed Hetlioz by his doctor.5 Like Ted, Ianto also faced disturbing and vivid dreams.5 He reported that while on Hetlioz, “I slept 12 hours – but it was not good sleep. I sleep 8 hours normally. I simply could not get out of bed, even after waking up at 6, 8, and 10 hours. I was beyond exhausted.”5 In both of these cases, taking Hetlioz amplified the burdens of Non-24 instead of alleviating them. Although Hetlioz was initially approved in 2014, the drug was recently recalled in early 2024 on the grounds of mislabeling, a lack of evidence for long-term efficacy, and the lack of subjective patient reported data in the clinical studies.7
Amid this backlash, other patients on WebMD reviews have reported life-changing effects with Hetlioz. Metalones, a 40 year-old mother, experienced both personal and social benefits after beginning Hetlioz, explaining “I was finally able to experience what it was like to be ‘normal’ and not be looked down on for being ‘irresponsible or lazy’.”5 She began homeschooling her daughter and making appointments earlier in the day to take care of herself and family, something she wasn’t able to do before, due to excessive exhaustion.5 When Hetlioz was recalled, Metalones’ insurance no longer covered the cost.5 With an out-of-pocket cost of approximately $19,000 per month, or $228,000 a year,6 Metalones couldn’t afford to pay for Hetlioz herself, so she had to stop taking it.5 Without Hetlioz, Metalones reported regression in her mental well-being, stating, “I’ve spiraled back down into severe depression and anxiety and stay in bed most of the day, because I’m too exhausted and apathetic to get up and do anything. I’m a shell of the person I used to be.”5
The misalignment of the external world with one’s internal rhythm in people with Non-24 introduces and reinforces an intense disconnect that must be bridged. Personalized approaches to manage Non-24, like free running and adjusted schedules, promise hope to some patients. However, successful deployment of these strategies depend greatly on the understanding and support of family and colleagues. Hetlioz has the potential to help, yet its benefits are diminished by the negative side effects, high cost, and lack of access. There are currently no other drugs approved for the treatment of Non-24, so more accessible treatments and improved technologies need to be developed in order to find an effective and sustainable solution. Management of Non-24 should not fall on the shoulders of patients alone. We all have a responsibility to develop a greater awareness of and accommodate those struggling with Non-24, so that this chronic separation from day and night does not cause a chronic separation from the world.
References
- Non-24-Hour Sleep-Wake Disorder. National Organization for Rare Disorders. (2023, November 20). https://rarediseases.org/rare-diseases/non-24-hour-sleep-wake-disorder/
- L. E. M. Miles et al., Blind Man Living in Normal Society Has Circadian Rhythms of 24.9 Hours. Science 198, 421-423 (1977). DOI:10.1126/science.910139
- Şahin, Z., Kalkan, Ö. F., & Aktas, O. (2022). How Does the Circadian Rhythm Function in Blind People Who Have No Light Perception?. Hipokrat Tıp Dergisi, 2(2), 38-46.
- Lockley, S. W., Dressman, M. A., Licamele, L., Xiao, C., Fisher, D. M., Flynn-Evans, E. E., … & Polymeropoulos, M. H. (2015). Tasimelteon for non-24-hour sleep–wake disorder in totally blind people (SET and RESET): two multicentre, randomised, double-masked, placebo-controlled phase 3 trials. The Lancet, 386(10005), 1754-1764.
- WebMD. (n.d.). Hetlioz oral reviews and user ratings: Effectiveness, ease of use, and satisfaction. WebMD. https://reviews.webmd.com/drugs/drugreview-165884-hetlioz-oral
- Tasimelteon Prices, Coupons, Copay Cards & Patient Assistance. Drugs.com. https://www.drugs.com/price-guide/tasimelteon
- The Food and Drug Administration. (2024, June 7). Federal Register :: Proposal to refuse to approve a new drug application supplement for hetlioz (tasimelteon); opportunity for a hearing. Federal Register. https://www.federalregister.gov/documents/2024/06/07/2024-12564/proposal-to-refuse-to-approve-a-new-drug-application-supplement-for-hetlioz-tasimelteon-opportunity
- Non-24-Hour Sleep-Wake Disorder. (2012, June 7). Living With Circadian Sleep Condition: Non-24-Hour Disorder. YouTube. https://www.youtube.com/watch?v=CqBaY8577cQ
